| |
|
|
BENIGN PAROXYSMAL POSITIONAL VERTIGO |
|
Benign paroxysmal positional vertigo (BPPV)
is one of the most common etiologies of peripheral vertigo. As the name implies,
the cause of vertigo is benign. Despite being of a benign etiology, this entity
can produce severely disabling symptoms of vertigo, nausea and vomiting, and
often brings a patient to the emergency room. Fortunately, BPPV can be diagnosed
clinically by a simple bedside maneuver and can be treated successfully using
non-pharmacological means in most cases. |
|
Epidemiology
Mean age of onset – 54 years (range 11-84 yrs)
Incidence – about 107 / 100,000 / year
Of patients referred to a speciality dizziness
clinic: about 17% have BPPV |
|
Pathophysiology
BPPV is caused by loose particle debris of otoliths, also known as otoconia.
Otoliths are normally attached to a membrane inside the utricle and saccule.
There are composed of calcium carbonate particles. Since they are denser than
the surrounding endolymph, when they break free, gravity pulls them downward
into the posterior semicircular canals of the vestibular labyrinth.
Otoliths may become displaced from the utricle by aging,
head trauma, or labyrinthine
disease. When this occurs, the otoliths almost always enter the
posterior semicircular duct since this is the most dependent of the three ducts.
Changing head position relative to gravity causes the free otoliths to
gravitate longitudinally through the canal. The concurrent flow of endolymph
stimulates the hair cells of the affected semicircular canal, causing vertigo. |
|
 |
Signs / Symptoms
•
Vertigo
Intermittent (paroxysmal)
Triggered by head movements (characteristically
occurs when rolling over in bed, leaning forward or turning the head
horizontally)
Usually lasts 10-20 seconds
•
Nystagmus
Fast phase will be toward the affected ear in BPPV
Mixed torsional and vertical components
Latency of a few seconds after provocative maneuver
•
Nausea, vomiting
Associated with vertigo |
Diagnosis
Diagnosis of benign paroxysmal positional vertigo (BPPV), the most common
cause of peripheral vertigo is made by observing the response to a bedside test
called the “Dix-Hallpike Maneuver” as
demonstrated below. |
|

|
|
(Figure Above) The Dix–Hallpike Test of a
Patient with Benign Paroxysmal Positional Vertigo Affecting the Right Ear.
In Panel A, the examiner stands at the patient's right side and rotates the
patient's head 45 degrees to the right to align the right posterior semicircular
canal with the sagittal plane of the body.
In Panel B, the examiner moves the
patient, whose eyes are open, from the seated to the supine right-ear-down
position and then extends the patient's neck slightly so that the chin is
pointed slightly upward. The latency, duration, and direction of nystagmus, if
present, and the latency and duration of vertigo, if present, should be noted.
The red arrows in the inset depict the direction of nystagmus in patients with
typical benign paroxysmal positional vertigo. The presumed location in the
labyrinth of the free-floating debris thought to cause the disorder is also
shown. Please note: this maneuver should not be performed in patients with
symptomatic cervical stenosis. Reproduced from Furman and Cass, Benign Paroxysmal Positional Vertigo,
NEJM Vol 341: 1590-1596,1999.
|
|
![]() |
(Above) Video of Nystagmus with BPPV [Place the cursor over the
box and the video will play]. This middle-aged woman
presented with a two week history of positional vertigo preceded by turning over
in bed onto the right side. Just prior to the onset of symptoms, she had
extensive dental work, lying fully recumbent in the dental chair for several
hours. On examination, when the right ear was placed in the dependent position
using the Dix-Hallpike maneuver, she developed a burst of nystagmus (shown in
this video). The nystagmus had slow phases directed downward with a torsional
component such that the poles of the eyes rotated toward the above (left) ear.
Correspondingly, the quick phases beat up and counter-clockwise (from the
examiner's vantage). The nystagmus appeared more vertical on left gaze and more
torsional on right gaze. This pattern of nystagmus is just as expected from
stimulation of the right posterior semicircular canal. The patient was relieved
of all symptoms following a particle repositioning maneuver. (Reproduced
with permission of the American Academy of Neurology).
|
The diagnostic criteria for BPPV are shown below:
|
|
 |
Reproduced from Furman and Cass, Benign Paroxysmal Positional Vertigo, NEJM. Vol
341: 1590-1596, 1999.
Treatment
The most effective treatment for BPPV is the Epley
Maneuver, with a success rate of about 80%. The purpose of this
maneuver is to reposition the loose endolymph crystals by a series of movement
which utilize changes in head position and the effect of gravity on the otoconia. |
|
|
|
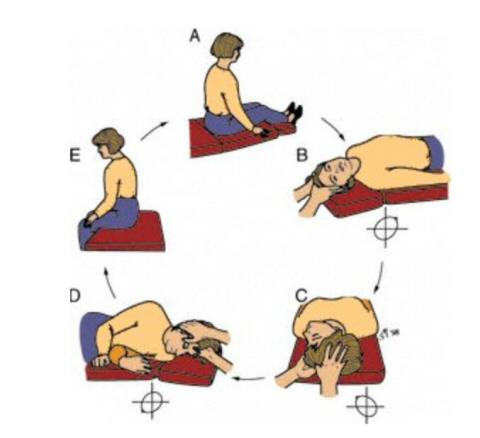
A) The patient starts upright
B) The patient leans backwards briskly
(with help of the clinician) and head turned 45 degrees so that the affected
ear, as previously determined by the Dix-Hallpike maneuver, is facing down
C) After the nystagmus stops (30-60
seconds) the patient is turned 90 degrees so that the opposite ear is now facing
down.
D) After about 30-60 seconds, the patient
turns the same direction into the lateral decubitus position so that nose faces
down
E) After about 30 seconds, the patient is
returned to the sitting position
The patient should be kept upright for the next 48 hours if possible, even
while sleeping. |
|
|
|