| |
|
|
COMMON ENTRAPMENT
NEUROPATHIES |
|
|
|
|
|
Median Neuropathy at the Wrist (Carpal Tunnel
Syndrome)
Carpal tunnel syndrome (CTS) is the most common of all entrapment
neuropathies.
Anatomy
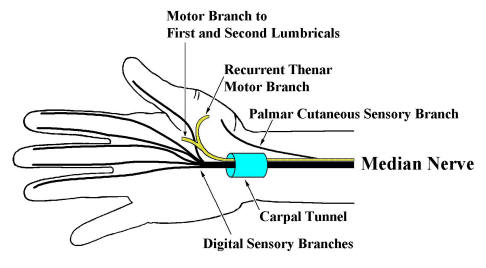
Just proximal to the wrist, the Palmar Cutaneous
Sensory branch leave the median nerve to run subcutaneously to supply
sensation over the thenar eminence. The median nerve then enters the wrist
through the carpal tunnel. Carpal bones make up the floor and sides of the
carpal tunnel, with the thick transverse carpal
ligament forming the roof. In addition to the median nerve, nine
flexor tendons traverse the carpal tunnel as well. In the palm, the median nerve
divides into motor and sensory divisions. The motor division travels distally
into the palm supplying the First and Second lumbricals. In addition, the Recurrent
Thenar Motor Branch is given off. This branch turns around (hence,
recurrent) to supply muscular branches to most of the thenar eminence including
the opponens pollicis, abductor pollicis brevis and superficial head of the
flexor pollicis brevis. The sensory fibers of the
median nerve that course though the carpal tunnel supply the medial thumb,
index, middle and lateral half of the ring finger.
|
|
|
|
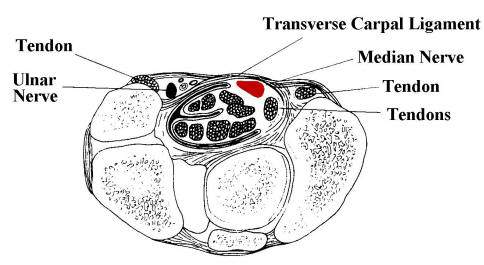
Above: cross sectional
anatomy through the wrist at the carpal tunnel (median nerve in red). |
|
Etiology
Most cases are idiopathic. In most cases, edema, vascular sclerosis and
fibrosis are seen, findings consistent with repeated stress to connective
tissue. Demyelination follows compression and ischemia of the median nerve, and
if severe enough, Wallerian degeneration and axonal loss ensue. Occupations or
activities which involve repetitive hand use clearly increase the risk of CTS.
Other predisposing etiologies include certain systemic disorders, most notably hypothyroidism,
rheumatoid arthritis and amyloidosis.
Clinical Presentation
Patients with CTS may present with a variety of symptoms and signs. Women are
more often affected than men. Although usually bilateral clinically and
electrically, the dominant hand is usually more severely affected, especially in
idiopathic cases. Patients complain of wrist and arm pain associated with
paresthesias in the hand. The pain may be localized to the wrist, or may radiate
to the forearm, arm or rarely the shoulder; the neck is not affected. Some
patients may describe a diffuse, poorly localized ache involving the entire arm.
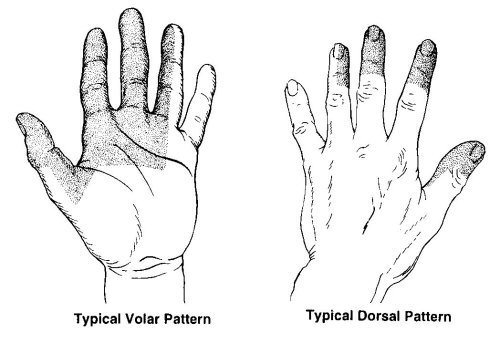
Paresthesias are frequently present in a median distribution (medial thumb,
index, middle and lateral ring finger). While many patients report that the
entire hand falls asleep, if asked directly about little finger involvement,
most will subsequently note that the little finger is spared.
|
|
 |
|
Above: typical
distribution of sensory symptoms in carpal tunnel syndrome. |
|
Symptoms are often provoked when either a flexed or extended wrist posture is
assumed. Most commonly, this occurs during ordinary activities, such as driving,
holding a phone, book or newspaper. Nocturnal
paresthesias are particularly common. During sleep, persistent wrist
flexion or extension leads to increased carpal tunnel pressure, nerve ischemia
and subsequent paresthesias. Patients will frequently awaken from sleep and
shake or ring out their hands, or hold them under warm running water.
Sensory fibers are involved early in the majority of patients. Pain and
paresthesias usually bring patients to medical attention. Motor fibers may
become involved in more advanced cases. Weakness of thumb abduction and
opposition may develop, followed by frank atrophy of the thenar eminence. Some
patients describe difficulty buttoning shirts, opening a jar, or turning a
doorknob. However, it is unusual to develop significant functional impairment
from loss of median motor function in the hand.
The sensory examination may disclose hypesthesia in the median distribution.
Sensation over the thenar area in spared, as this area is innervated by the
Palmar Cutaneous Sensory Branch, arising proximal to the carpal tunnel. The Tinel's
sign, tested by tapping over the median nerve at the wrist, and the Phalen's
maneuver, holding the wrist passively flexed, may both provoke
symptoms.
The motor examination involves inspection of the hand looking for wasting of
the thenar eminence (severe cases) and testing the strength of thumb abduction
and opposition.
|
|
 |
|
Ulnar Neuropathy at the Elbow
Ulnar neuropathy at the elbow (UNE) is second only to
median nerve entrapment at the wrist (i.e., carpal tunnel syndrome) as the most
common entrapment neuropathy affecting the upper extremity. Lesions of the lower
brachial plexus or C8-T1 roots may result in similar symptoms to UNE.
Anatomy
The ulnar nerve is essentially derived from the C8
and T1 roots. All ulnar fibers travel through the lower
trunk of the brachial plexus and then continue into the medial
cord. The terminal extension of the medial cord becomes the ulnar
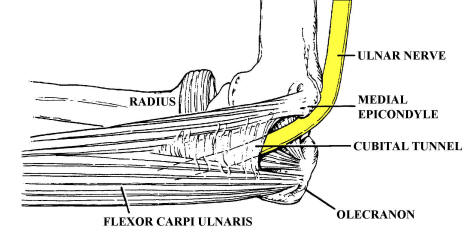
nerve. The ulnar nerve then travels medially and distally toward the elbow. At
the elbow, the nerve enters the ulnar groove
formed between the medial epicondyle and the olecranon process. Slightly distal
to the groove in the proximal forearm, the ulnar nerve travels under the
tendinous arch of the two heads of the flexor carpi ulnaris muscle, known as the
humeral-ulnar aponeurosis (HUA) or "cubital
tunnel." Muscular branches to the flexor carpi ulnaris and the
medial division (fourth and fifth digits) of the flexor digitorum profundus are
then given off.
The nerve then descends through the medial forearm, giving off no further
muscular branches until after the wrist. Slightly proximal to the wrist, the
dorsal ulnar cutaneous sensory branch exits to supply sensation to the dorsal
medial hand and the dorsal fifth and medial fourth digits. The nerve next enters
the medial wrist to supply sensation to the volar fifth and medial fourth digits
and muscular innervation to the hypothenar muscles, the palmar and dorsal
interossei, the third and fourth lumbricals, and two muscles in the thenar
eminence, the adductor pollicis and the deep head of the flexor pollicis brevis.
|
|
Etiology
UNE usually occurs as a result of chronic mechanical compression or stretch,
either at the groove or at the cubital
tunnel. Although rare cases of ulnar neuropathy at the groove are
caused by ganglia, tumors, fibrous bands, or accessory muscles, most
are caused by external compression and repeated trauma. Elbow
fracture, often years before, and subsequent arthritic change of the elbow joint
may result in so-called tardy ulnar palsy.
In addition, chronic minor trauma and compression (including leaning on the
elbow) can either exacerbate or cause ulnar neuropathy at the groove. Ulnar
neuropathy at the groove is also common in patients who have been immobilized
because of surgery or who sustain compression during anesthesia or coma.
Distal to the groove is the cubital tunnel,
the other major site of compression of the ulnar nerve in the region of the
elbow. Although some use the term cubital tunnel syndrome to refer to all
lesions of the ulnar nerve around the elbow, it more properly denotes
compression of the ulnar nerve under the HUA. Some individuals have congenitally
tight cubital tunnels that predispose them to compression. Repeated
and persistent flexion stretches the ulnar nerve and increases the
pressure in the cubital tunnel, leading to subsequent ulnar neuropathy.
|
|
Clinical Presentation
UNE caused by compression at the groove or at the cubital tunnel may present
in a similar manner. In contrast to carpal tunnel syndrome in which sensory
symptoms predominate, motor symptoms are more common in ulnar neuropathy,
especially in chronic cases. In some patients, insidious motor loss may occur
without sensory symptoms, particularly in those with slowly worsening mechanical
compression. As most of the intrinsic hand muscles are ulnar innervated,
weakness of these muscles leads to loss of dexterity and to decreased grip and
pinch strength. These are often the complaints that bring the patient to medical
attention. There may be atrophy of both the hypothenar and thenar eminences (the
ulnar-innervated adductor pollicis and deep head of the flexor pollicis brevis
are in the thenar eminence). However, thumb abduction is spared (median and
radial innervated).
|
|
|
|
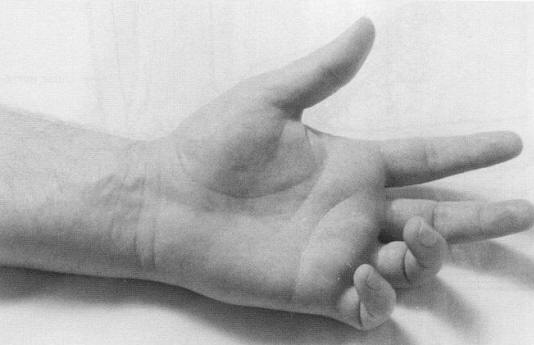
In moderate or advanced cases, examination often shows the classic hand
postures that occur with ulnar muscle weakness. The most recognized is the "Benediction
posture" (see photo above). The ring and little fingers are clawed, with the metacarpophalangeal joints hyperextended and the proximal and distal
interphalangeal joints flexed (from third and fourth lumbrical weakness), while
the fingers and thumb are held slightly abducted (from interossei and adductor
pollicis weakness). Patients with ulnar neuropathy may not be able to flex the
distal fourth and fifth fingers completely when making a grip; in contrast, the
median-innervated second and third distal digits flex normally.
In UNE, sensory disturbance, when present, involves the volar and dorsal
fifth and medial fourth digits, and the medial hand. The sensory disturbance
does not extend proximally much beyond the wrist crease. Sensory involvement
extending into the medial forearm implies a higher lesion in the plexus or nerve
roots (i.e., this is the territory of the medial antebrachial cutaneous sensory
nerve, which arises directly from the medial cord of the brachial plexus).
Pain, when present, may localize to the elbow or radiate down to the medial
forearm and wrist. Paresthesias may be reproduced by placing the elbow in a
flexed position or by applying pressure to the groove behind the medial
epicondyle. The ulnar nerve may be palpably enlarged and tender. Especially in
patients with ulnar neuropathy at the cubital tunnel, the nerve may be palpably
taut with decreased mobility.
|
|
 |
|
Radial Neuropathy at the Spiral Groove
Of the major upper extremity nerves, compression of the
radial nerve is less common. However, the radial nerve is susceptible to
external compression and can result in a classic syndrome of wrist and finger
drop.
Anatomy
The radial nerve receives innervation from all three
trunks of the brachial plexus and, correspondingly, a contribution from each of
the C5-T1 nerve roots. After each trunk divides into an anterior and posterior
division, the posterior divisions from all three trunks unite to form the
posterior cord. The posterior cord
gives off the axillary, thoracodorsal, and subscapular nerves before becoming
the radial nerve. In the high arm, the radial nerve first supplies the three
heads of the triceps brachia before wrapping around the posterior hummers in the
spiral groove.
Descending into the region of the elbow, muscular branches are then given off to
the brachioradialis, and then all the extensors of the wrist and fingers. In
addition, the superficial radial sensory nerve is given off to supply sensation
over the lateral dorsum of the hand as well as part of the thumb and the dorsal
proximal phalanges of the index, middle, and ring fingers.
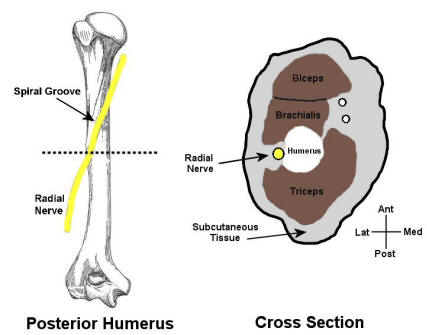
Etiology
The most common radial neuropathy occurs at the spiral groove. Here, the
nerve lies juxtaposed to the hummers and is quite susceptible to compression,
especially following prolonged immobilization (see figure above). One of the
times this characteristically occurs is when a person has draped an arm over a
chair or bench during a deep sleep or while intoxicated ("Saturday
night palsy"). The subsequent prolonged immobility results in
compression and demyelination of the radial nerve.
Clinical Presentation
Clinically, marked wrist drop and finger drop develop in radial neuropathy at
the spiral groove. Notably, elbow extension (triceps) is spared. Sensory
disturbance is present in the distribution of the superficial radial sensory
nerve, consisting of altered sensation over the lateral dorsum of the hand, part
of the thumb, and the dorsal proximal phalanges of the index, middle, and ring
fingers.
|
|
 |
|
Personal Neuropathy at the Fibular Neck
Peroneal neuropathy often occurs from compression at
the fibular neck, where the nerve is quite superficial and vulnerable to injury.
Patients usually present with a footdrop and sensory disturbance over the
lateral calf and dorsum of the foot. However, patients with sciatic neuropathy,
lumbosacral plexopathy, or L5 radiculopathy may present with a similar pattern
of numbness and weakness.
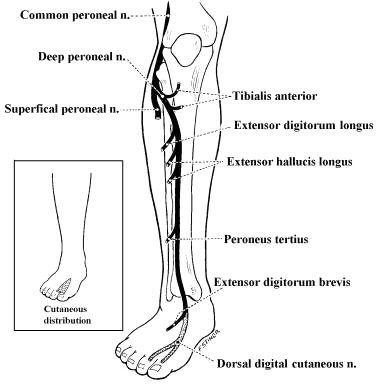
Anatomy
The peroneal nerve is derived predominantly from the L4-S1 nerve roots, which
travel through the lumbosacral plexus and eventually the sciatic nerve. Within
the sciatic nerve, the fibers that eventually form the common
peroneal nerve run separately from those that distally become the
tibial nerve. The sciatic nerve bifurcates above the popliteal fossa into the
common peroneal and tibial nerves. The common peroneal nerve winds around the
fibular neck and passes through the fibular tunnel between the peroneus longus
muscle and the fibula. The common peroneal nerve then divides into superficial
and deep branches. The deep peroneal nerve
innervates the dorsiflexors of the ankle and toes. It also supplies sensation to
the web space between the first and second toes. The superficial
peroneal nerve innervates the ankle evertors and then supplies
sensation to the mid- and lower lateral calf.
Etiology
Peroneal neuropathy can be seen as a result of a variety of conditions. Acute
peroneal neuropathy often follows trauma, forcible
stretch injury, or compression from
prolonged immobilization. In the hospital, this occurs most often
postoperatively in patients who have received anesthesia or heavy sedation.
Slowly progressive lesions often suggest a mass lesion, such as a ganglion or
nerve sheath tumor. Entrapment of the peroneal nerve at the fibular tunnel,
although quite uncommon, may also present in a progressive manner.
Several other circumstances predispose one to peroneal neuropathy. Habitual
leg crossing may repetitively injure the peroneal nerve at the
fibular neck, where it is quite superficial. Similarly, repetitive
stretch from squatting, for example, by gardeners has also been
associated with peroneal neuropathy. In addition, patients who are thin or who
have recently lost a substantial amount of weight
may be prone to peroneal palsy, probably because of the lack of protective
supporting adipose tissue at the fibular neck.
Clinical Presentation
Patients with peroneal neuropathy at the fibular neck present with a
characteristic neurologic picture. Most often, both the deep and superficial
peroneal nerves are affected. Involvement of the deep peroneal nerve leads to
weakness of toe and ankle dorsiflexion, resulting in a foot
and toe drop. Dysfunction of the superficial peroneal nerve results
in weakness of foot eversion. Clinically, weakness of these muscles results in a
stereotyped set of symptoms. Patients note a slapping quality of their foot as
it hits the ground while walking. Weakness of eversion leads to a tendency to
trip, especially on uneven sidewalks or curbs, and an increased risk of sprained
ankles. When observed while walking, patients have a so-called "steppage
gait" whereby they bring their knee up higher than usual so that
the dropped foot clears the floor.
Sensory disturbance develops over the mid- and lower lateral calf and the
dorsum of the foot. Local pain and a Tinel's sign may be present over the
lateral fibular neck. In isolated peroneal neuropathy at the fibular neck,
function of the sciatic, tibial, and sural nerves remains normal. Most
important, ankle inversion is spared, mediated by the tibialis posterior (L5,
sciatic-tibial nerve). Finally, all reflexes, including the ankle reflex, remain
normal in an isolated peroneal neuropathy.
It is important to note that lesions of the sciatic nerve, lesions of the
lumbosacral plexus, and L5 radiculopathy may also present with a footdrop and
numbness over the lateral calf and dorsum of the foot. Indeed, these lesions,
especially early on, occasionally mimic a peroneal palsy almost exactly,
including abnormalities of sensation. It is in these cases that EMG studies are
especially helpful.
|
|
|
|
Lateral Femoral Cutaneous Sensory Neuropathy (Meralgia
Paresthetica)
Entrapment of the lateral femoral cutaneous sensory
nerve is the most common entrapment neuropathy in the lower extremity. It is
associated with a classic clinical syndrome, known as meralgia
paresthetica.
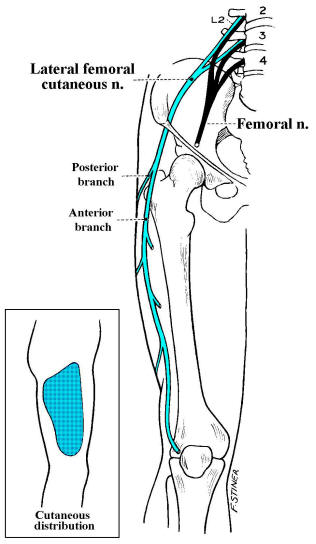
Anatomy
The lateral femoral cutaneous nerve is a pure sensory nerve that is derived
from the L2-L3 roots and runs under the inguinal
ligament near the superior iliac spine, where it may be injured or
entrapped. The lateral femoral cutaneous nerve only supplies sensation to a
large oval area of skin over the lateral and anterior thigh.
Etiology
This entrapment is more common in patients who are obese,
wear tight underwear or pants, or who have diabetes.
Although the vast majority of cases are due to an entrapment at the inguinal
ligament, rare cases have resulted from tumors and other mass lesions
compressing the upper lumbar plexus more proximally.
Clinical Presentation
The clinical syndrome, known as meralgia
paresthetica, results in a painful, burning, numb patch of skin over
the anterior and lateral thigh, sometimes worst in the standing position.
Because there is no muscular innervation from this nerve, there is no associated
muscle atrophy, weakness, or loss of reflexes. |
|
|
|