| |
|
|
Hypertensive Intracerebral Hemorrhage:
Common Locations and Clinical Signs |
|
 |
|
Spontaneous intracerebral hemorrhage (ICH) refers to bleeding into the
parenchyma of the brain and/or ventricles, excluding trauma as an etiology. The
incidence is about 37,000-52,000 cases / year in the US. Although accounting for
only 10-15% of strokes, the dire clinical consequences of spontaneous ICH make
its early recognition especially important. The one-year mortality rate of about
62 percent greatly exceeds that of ischemic stroke.
Hypertension is the etiology in the majority of spontaneous intracerebral
hemorrhages. The diagnosis of hypertensive ICH is suggested by a
clinical history of hypertensive disease and imaging studies that demonstrate
hemorrhage in a typical location. In some cases, it may be necessary to do
further studies, including angiography to exclude other causes of ICH. Some
other causes of ICH include: amyloid angiopathy,
arteriovenous malformation
(AVM), intracranial aneurysm,
angiomas, neoplasm,
venous sinus thrombosis, coagulopathy,
vasculitis, cocaine and hemorrhagic conversion of ischemic stroke.
|
|

|
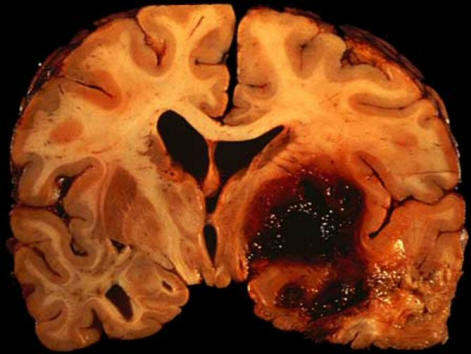
Figure above: Hypertensive intracerebral hemorrhages most
commonly involve the basal ganglia,
originating from ascending lenticulostriate branches of the middle cerebral
artery (B); the thalamus, originating from ascending thalmogeniculate branches
of the posterior cerebral artery (C); the pons, originating from paramedian
branches of the basilar artery (D); and the cerebellum, originating from
penetrating branches of the posterior inferior, anterior inferior, or superior
cerebellar arteries (E). Less common is involvement of the cerebral lobes,
originating from penetrating cortical branches of the anterior, middle, or
posterior cerebral arteries (A). From Qureshi et al. Spontaneous Intracerebral
Hemorrhage, NEJM. 344 (19): 1450, Figure 2. May 10, 2001
|
CLINICAL PRESENTATION
Symptoms and signs of hypertensive ICH depend on location affected.
The most
common locations of hypertensive ICH are: 1) Basal ganglia (putamen or caudate),
2) Thalamus, 3) Pons and 4) Cerebellum. Within the basal ganglia region, it is rare for an ICH to specifically affect one area; thus an overlapping of clinical
signs/symptoms usually occurs. Rarely, hypertensive ICH can occur as a lobar
hemorrhage (“A” in the figure above).
|
|
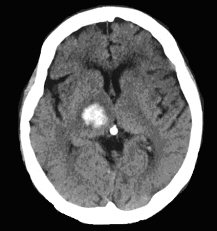
BASAL GANGLIA: PUTAMEN |
 |
The putamen is the most common site for hypertensive ICH
(35%).•
Headache, nausea and vomiting
•
Contralateral hemiparesis: progressive usually starting with face, then arm and
leg
• Contralateral hemisensory loss
• May have aphasia if dominant side affected, or neglect if non-dominant lesion
• Contralateral Babinski sign, or may develop bilateral Babinski signs later.
• Dysarthria
• Eyes deviate toward side of the lesion
• Depressed level of consciousness: depends on size of hematoma
• If large hematoma, brainstem signs develop and death ensues
Note:
the signs and symptoms of an ICH in the basal ganglia are very similar to those
from an MCA ischemic stroke.
|
|
BASAL GANGLIA: CAUDATE |
 |
|
• Headache, nausea and vomiting
• Meningismus: including severe headache and nuchal rigidity 2nd to close
proximity to lateral ventricle
• Marked confusion
•
Abulia (lack of drive)
• Contralateral conjugate eye deviation
• Mild contralateral hemiparesis
|
|
THALAMUS |
 |
|
•
Headache, nausea and vomiting
•
Prominent contralateral hemisensory loss
• Variable contralateral hemiparesis (depends on internal capsular involvement)
• Contralateral homonymous hemianopia (parietal-temporal involvement)
•
Impaired vertical gaze
• Hyperconvergent eyes (depends on dorsal midbrain involvement
• Miotic pupils
• Transient aphasia with dominant lesion, or neglect with non-dominant lesion
• Early depressed level of consciousness (due to involvement of the reticular
activating system)
|
|
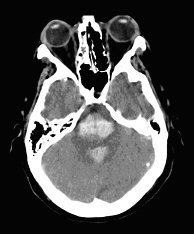
PONS |
|
|
•
Early coma
•
Pin-point minimally reactive pupils
(remember 4 P's - pons, pinpoint,
pupils)
• Bilateral Babinski signs
•
Impaired horizontal gaze
•
Quadriparesis
• Facial weakness
|
|
CEREBELLUM |

|
• Headache, nausea and vomiting (often occipital headache)
• Truncal and gait ataxia
Cerebellar ICH is a neurosurgical emergency!
If the hemorrhage or surrounding swelling enlarges, there can be direct
compression on the brainstem and/or 4th ventricle. Obstruction of the 4th
ventricle then results in acute hydrocephalus. Depressed level of consciousness
follows that rapidly progresses to coma, herniation and death. This is a
treatable condition surgically if recognized. Too often, cerebellar ICH is
misinterpreted as the "flu" or gastroenteritis. Despite affecting the cerebellum,
it is uncommon to see classic ataxia on finger-to-nose, or heel-to-skin testing.
The key physical exam finding is gait ataxia.
|
|
LOBAR |
 |
|
The symptoms and signs of a hypertensive ICH essentially mimic those of
occlusions of the major branches of the
anterior and posterior circulation
(i.e., anterior
cerebral, middle cerebral and posterior cerebral arteries).
Prominent nausea and vomiting in the setting of any focal neurologic deficit
suggest the possibility of accompanying increased intracranial pressure, as
often occurs with ICH.
Of all the hypertensive ICH locations, it is the least common. Even in a
hypertensive patient, this diagnosis is one of exclusion. Patients with lobar
ICH all require further investigation looking for an underlying structural lesion (e.g., AVM,
tumor, etc.)
|
|
|
|