| |
|
|
LOWER MOTOR NEURON LESIONS |
|
Motor System Overview
The command to contract a muscle voluntarily is initiated in the cerebral
cortex and is transmitted through only two synapses. The cortical neuron is
called the upper motor neuron. The first
synapse is upon the lower motor neuron,
whose cell body lives in the spinal cord. The second synapse is the
neuromuscular junction itself. This direct pathway is collectively called the
pyramidal system (after the microscopic
appearance of the neuron cell bodies in the cortex).
Other circuitry involved in motor function includes loops through the basal
ganglia and thalamus, or to the pons and cerebellum and thalamus. These
extrapyramidal circuits are more complex and do
not directly activate muscle contraction, but are essential to the proper
functioning of the pyramidal output system.
Lesions of the pyramidal system are divided into upper and lower motor neuron
types. Lesions of the basal ganglia or cerebellum are neither upper nor lower
motor neuron lesions.
|
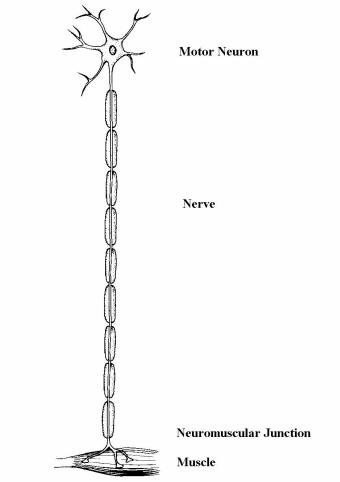
Left: the lower motor neuron includes the
anterior horn cell (motor neuron), nerve, neuromuscular junction, and muscle. |
Lower Motor Neuron
Lesions
• Anatomy. Cell bodies are located in
anterior horn of the spinal cord. Axons emerge in the ventral roots and then
continue as peripheral nerves.
• LMN Syndrome. Lesions of the cell body
or (more commonly) the axon produce a classic LMN syndrome. Corresponding
sensory loss and the anatomic distribution of the weakness are usually the best
clues to aid localization further.
Weakness. LMN lesions produce weakness, similar to UMN lesions.
However, the anatomic patterns are different. In LMN lesions, weakness often
fits a pattern of muscles supplied by the same nerve root (myotomal pattern) or
same peripheral nerve. Another common LMN pattern is the length dependent
pattern (i.e., the longest nerves are affected the most). This pattern, the
stocking-glove pattern, is typically seen in peripheral neuropathies.
Hyporeflexia. In LMN lesions, reflexes are typically reduced or
absent in the distribution of the weakness. Caution - reflexes can be reduced
initially in severe or acute UMN lesions.
Flaccidity. Muscle tone is typically reduced. In extreme cases,
muscle tone is completely flaccid.
|
 |
 |
|
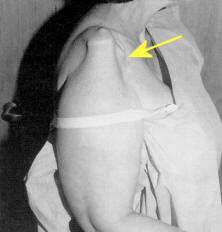
Atrophy (see figures above). Some muscle atrophy occurs in any lesion resulting in
weakness from disuse. However, in many LMN lesions, the atrophy is pronounced.
It is best to look for atrophy in distal muscles (not covered by adipose) (see
figure upper left) or
muscle adjacent to bony structures (see figure upper right).
Fasciculations result from loss of innervation to muscle. They
indicate damage either in the anterior horn cell or axon. They are recognized as
a brief muscle twitch. Note: everyone has some normal, so-called benign
fasciculations. However, when fasiculations are prominent or seen in the
distribution of other LMN signs, they are supportive of an LMN lesion.
|
One Other Important Note About LMN Syndromes.
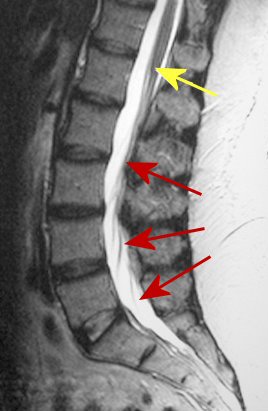
The central nervous system is comprised of the brain and spinal cord. Often,
the terms spinal cord and spine are used interchangeably - they are not. The
spinal cord terminates at L1 in adults (yellow arrow below). Any lesion above
this point will result in an UMN syndrome. However, at this point and below
(cauda equina) is the LMN (red arrows). Thus, a lesion in the lumbar spine
results in a LMN syndrome, but never an UMN syndrome.
Don't make the mistake of ordering an MRI of the lumbar spine for a patient with
weakness of the legs, hyperreflexia and extensor plantar responses.
|
|
|
|
|
|