Large Vessel Stroke
in the Anterior Circulation |
|
A stroke may result from occlusion of a vessel in the
anterior or posterior circulation of the brain with
varying clinical manifestations. This learning objective
first defines the arterial vessels that comprise the
anterior circulation of the brain.
It then reviews the clinical manifestations of stroke
resulting from occlusion of each of these vessels. It is
important to contrast these clinical manifestations with
those involving strokes of the posterior circulation, as
the etiology and treatment may differ. For this
information, please refer to the next learning objective,
large vessel strokes of the
posterior circulation.
A large vessel stroke of the anterior circulation
occurs when either a carotid
artery or a large arterial branch of a
carotid artery including the
middle or anterior cerebral arteries are
blocked. The resulting clinical manifestations, depend
on the vascular territory supplied by the blocked
artery, as well as the degree of collateral vessels
helping to perfuse the given area of brain. The carotid
arteries stem from the aortic arch. In the neck, they
bifurcate into the internal and external carotids. In
the brain, at the “Circle of
Willis” the internal carotid artery branches
into the middle cerebral artery and the anterior
cerebral artery. The anterior cerebrals may communicate
via the anterior communicating artery. In a small
percentage of people, the posterior cerebral artery also
stems from the anterior circulation. Remember, that the
anterior circulation usually connects to the posterior
circulation via the posterior communicating artery. Only
about 20% of the population has a complete “Circle of
Willis.” Please refer to the diagrams below to review
the cerebral blood supply and the cortical areas
supplied.
|
|
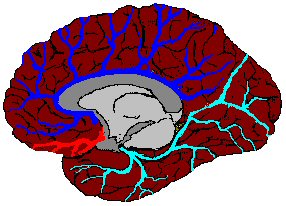
Medial View
of the Brain |
|
 |
|
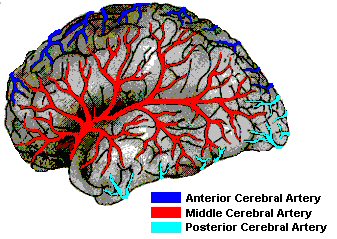
Lateral View
of the Brain |
|
|
 |
MRA of the Aortic Arch with Contrast Bolus.
(1) Aortic arch; (2) Brachiocephalic artery; (3) Right
Subclavian artery; (4) Left Subclavian artery; (5) Left
Common Carotid artery; (6) Right Common Carotid artery;
(7) Left Vertebral artery; (8) Left Common Carotid
artery; (9) Left Carotid Bifurcation; (10) Right
Vertebral artery; (11) Right Carotid Bifurcation; (12)
Right Internal Carotid artery; (13) Left Internal
Carotid Artery; (14) Left External Carotid artery; (15)
Right External Carotid artery; (16) Basilar artery; (17)
Right Internal Carotid artery (intracranial); (18) Left
Internal Carotid artery (intracranial); (19) Top of the
Basilar artery; (20) Vertebral arteries; (21) Vertebral
arteries
|
|
 |
MRA of the Neck - Extracranial Large Vessels.
ECA - External Carotid Artery; ICA - Internal Carotid
Artery; CCA - Common Carotid Artery; Vert - Vertebral
Artery
|
|
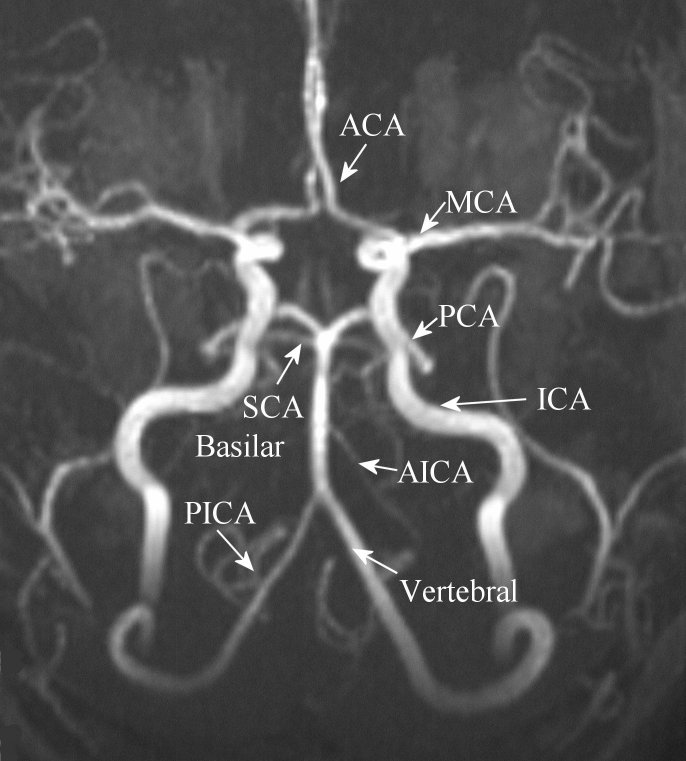 |
Magnetic Resonance Angiography (MRA) Intracranial
Study. ACA - anterior cerebral artery; MCA - middle
cerebral artery; PCA - posterior cerebral artery; SCA -
superior cerebellar artery; AICA - anterior inferior
cerebellar artery; PICA - posterior inferior cerebellar
artery
|
The next part of this learning objective will review the
major clinical manifestations of different types of
large vessel anterior circulation including the
anterior cerebral,
middle cerebral and
internal carotid
arteries.
|
|

Anterior Cerebral Artery
Stroke |
|
Incidence:
Relatively rare. ACA strokes make up only 0.6-3.0% of
acute ischemic strokes if vasospasm, or aneursymal
causes are excluded.
Etiologies:
Most
often embolic from heart, aorta or the internal carotid
artery. Rarely, due to intrinsic atherosclerotic disease
of the ACA. |

Note that the lower extremity resides on the
homunculus over the medial brain, in the distribution of
the ACA. |
Major Signs/Symptoms:
Contralateral leg
weakness / sensory impairment
Akinetic mutism (abulia) – a state of severely limited
responsiveness to the environment in the absence of
gross alteration of sensorimotor mechanisms.
Disturbance of judgment and/or emotion
Transcortical motor aphasia (with dominant lesions)
Non-dominant limb apraxia (with dominant lesions)
Urinary
dysfunction
|
|

Middle
Cerebral Artery
Stroke |
|
The MCA is the largest of the intracranial cerebral
vessels arising from then internal carotid artery.
The MCA first supplies deep penetrators to the basal
ganglia and internal capsule. In the Sylvian Fissure,
the MCA typically bifurcates in a Superior and Inferior
Division. The Superior Division supplies the lateral
Frontal and Parietal lobes, while the Inferior Division
supplies the Temporal and Posterior Parietal Lobes. |
|
Incidence:
Very common, especially strokes in the Superior
Division.
Etiologies:
Most
often embolic from heart, aorta or the internal carotid
artery. Rarely, due to
intrinsic atherosclerotic disease
of the MCA.
|

Note that the upper extremity, face and bulbar
muscles resides on the
homunculus over the lateral brain, in the distribution of
the MCA. |
|
|

Superior Division
MCA |
Major Signs/Symptoms:
Contralateral
hemiplegia, usually face and arm > leg
Contralateral sensory loss (esp. cortical sensory - two
point discrimination, graphesthesia, stererognosia, etc.)
Contralateral homonymous hemianopia (predominantly lower
quadrant)
Gaze
preference to the ipsilateral side of stroke
Aphasia, expressive (dominant hemisphere)
Neglect
syndrome (non-dominant hemisphere)
|
|

Inferior Division
MCA |
Major Signs/Symptoms:
Contralateral
homonymous superior quadrantanopsia
Aphasia, receptive (dominant hemisphere)
Constructional apraxia (non-dominant hemisphere)
Behavioral disturbance (non-dominant hemisphere)
|
|

Proximal Stem of
the MCA |
Major Signs/Symptoms:
Contralateral
hemiplegia, usually face = arm = leg (the leg is
involved as the internal capsule is affected as well)
Contralateral sensory loss (esp. cortical sensory - two
point discrimination, graphesthesia, stererognosia,etc.)
Contralateral homonymous hemianopia
Gaze
preference to the ipsilateral side of stroke
Aphasia, global (dominant hemisphere)
Neglect
syndrome (non-dominant hemisphere)
High
risk of increased intracranial pressure,
herniation and
death
|
|

Internal Carotid
Artery
Stroke |
|
The clinical manifestations of ICA stroke overlap with
those of the ACA and MCA. The deficits seen can vary
from minor, if good collateral flow exists, to a massive
infarction causing rapid cerebral edema, herniation and
death.
The only way to differentiate clinically if a stroke
is secondary to ICA stroke versus MCA stroke would be a
history of amaurosis fugax (transient visual loss in one
eye). This occurs due to disruption of blood flow in the
ophthalmic artery, a branch of the ICA. |

View of the Optic Fundus.
Note the cholesterol embolus in one the retinal
arteries. In patients with amaurosis fugax (transient
monocular blindness), the symptoms may result from
hemodynamic hypoperfusion or from emboli, as the case
here. |
Etiologies:
ICA stroke is most
commonly due to
atherosclerotic disease of the
vessel near its origin at the bifurcation
of the common carotid artery.
Rarely,
a
large embolus from the heart or
aortic arch can occlude the ICA
In
young patients without stroke risk factors, also
consider
carotid dissection,
especially in the setting of trauma, neck pain, or
especially if a Horner’s syndrome is present. The latter
occurs from disruption of sympathetic fibers that travel
in the carotid sheath. |
Major Signs/Symptoms:
See above lists for
ACA and MCA stroke
Rarely,
symptoms referable to the
Posterior Cerebral Artery (PCA),
can occur with carotid disease as 20% of
the population has a “fetal origin PCA” where the PCA
originates directly from the carotid via a large
posterior communicating artery and not from the top of
the basilar artery. |