|
Clinical
Differentiation Between
Thrombotic
and Embolic Stroke
|
|
This learning objective discusses how to clinical differentiate between a
thrombotic versus an embolic stroke. This distinction is important as it
provides valuable information on the potential etiology of stroke and can help
guide the diagnostic workup and management of a patient.
A thrombotic stroke occurs when a clot forms
at the site of a diseased blood vessel, due to pathological factors related to
the vessel. The underlying process is usually atherosclerosis and associated
chronic inflammation. Eventually a critical point is reached where the plaque
may rupture and triggers a inflammatory cascade that recruits platelets and
subsequent fibrin formation within the lumen of a vessel. The result is
disruption of blood flow to the brain supplied distally by the vessel, and a
subsequent stroke.
|
|
|
|
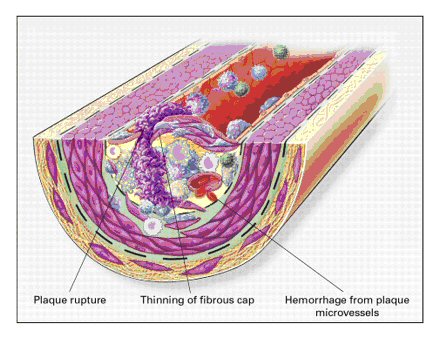
Unstable Fibrous Atherosclerotic
Plaque
Above: Rupture of the fibrous cap or ulceration of the fibrous plaque can
rapidly lead to thrombosis and usually occurs at sites of thinning of the
fibrous cap that covers the advanced lesion. Thinning of the fibrous cap is
apparently due to the continuing influx and activation of macrophages, which
release metalloproteinases and other proteolytic enzymes at these sites. These
enzymes cause degradation of the matrix, which can lead to hemorrhage from the
vasa vasorum or from the lumen of the artery and can result in thrombus
formation and occlusion of the artery. Adapted from: Ross, R, Atherosclerosis —
An Inflammatory Disease, NEJM, Volume 340:115-126, Figure 4, January 14, 1999. |
|
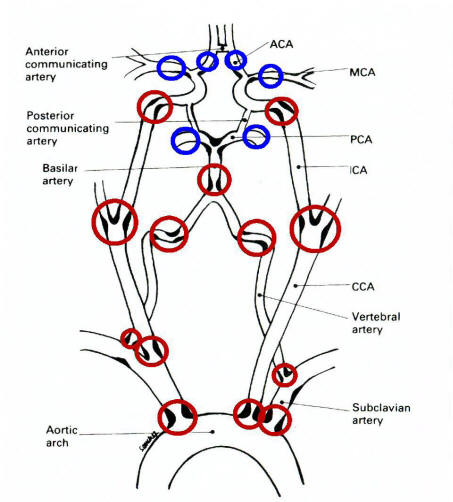 |
Above: Common locations for thrombosis.
Thrombosis most commonly occurs at sites of arterial atherosclerosis, typically
at the origin and bifurcation of vessels. The red circles indicate the most
common sites. The blue circles (intracranial MCA, ACA and PCA) are uncommonly
affected except in the Asian and African American populations. Adapted from
Caplan, Caplan's Stroke: A Clinical Approach, Third Edition, 2000. MCA = middle
cerebral artery; ACA = anterior cerebral artery; PCA = posterior cerebral
artery; ICA = internal carotid artery; CCA = common carotid artery.
|
|
An embolic stroke occurs when a clot formed in a proximal site in the
vasculature, moves downstream and lodges in a relatively random blood vessel and
infarcting brain tissue. Note that an embolus usually lodges in a previously
normal blood vessel, whereas a thrombus occurs in a diseased vessel.
|
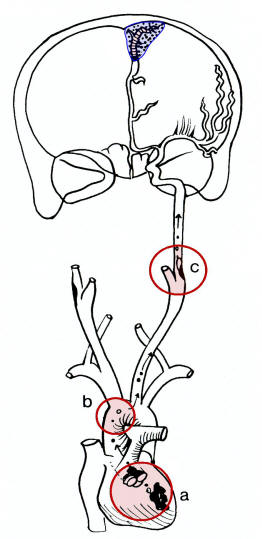
Common Sources of Emboli
Emboi most commonly orginate from the heart (a); aorta (b) or proximal
arteries (c); the latter known as artery-to-artery embolus. The embolus
then travels downstream and often occludes the anterior cerebral, middle
cerebral or posterior artery, or branch of one those arteries. Note: embolic
infarction are often wedged shaped (blue area). Adapted from Caplan, Caplan's
Stroke: A Clinical Approach, Third Edition, 2000. |
|
The following table lists general rules that help distinguish thrombotic versus
embolic strokes. Please keep in mind that many exceptions occur.
|
|
|
THROMBOTIC |
EMBOLIC
|
|
Risk Factors: |
Hypertension
Hyperlipidemia
Diabetes Mellitus
Smoking
Obesity
Other systemic atherosclerosis
Hypercoagulable states
|
Atrial fibrillation
Hypercoagulable states
Endocarditis
Dilated cardiomyopathy
Recent MI
Akinetic Heart segment
Prosthetic heart valve
Rheumatic heart disease
PFO / ASD
|
|
Etiologies: |
Large vessel:
Atherosclerosis
Small penetrating arteries:
Lipohylanosis
Rarely (vasculitis, dissection, hypercoagulable states)
|
Cardiac source
Artery-to-artery embolus
Right-Left Cardiac or Pulmonary Shunt
|
|
Clinical presentation: |
TIA symptoms frequent and occur in same
distribution
Symptoms may progress over minutes to hours
Symptoms may wax and wane
May occur during sleep and noticed on waking.
Associated seizures rare
|
TIAs may occur in different distributions
Maximal deficits at onset
Occurs anytime of day or night
May occur during vigorous activity
Seizures more likely associated |
|
Physical exam: |
May have
cortical or subcortical findings
May have a classic lacunar syndrome
|
Usually has
cortical findings |
|
Distributions: |
Most Common:
Internal carotid artery
Origin of the vertebral artery from the subclavian
Intracranial vertebral
Proximal and mid-basilar
Small penetrating arteries
(e.g., lenticulostriates of MCA and thalmoperforators from the proximal PCA)
MCA, PCA, ACA intracranial stenosis (uncommon except in Asian and African
American population)
|
Most Common:
MCA (stem or cortical branch)
PCA (stem or cortical branch)
ACA (stem or cortical branch)
Top of the Basilar
Lacunar syndrome uncommon
Rarely (PICA, AICA or SCA) |
|
Acute Treatment: |
Possible thrombolysis
|
Possible thrombolysis
|
|
Chronic Treatment: |
Usually antiplatelets
Possible carotid endartectomy for ICA high grade stenosis
Possible stenting (if accessible)
Risk factor modification
|
Often anticoagulation
with warfarin for definite cardioembolic source
Antiplatelets, if no definite embolic source discovered or if contraindicated
Surgical correction of PFO / ASD (selected cases) |