A 39 year-old woman presented with headaches, paranoid thinking, and hearing loss over 4 weeks.
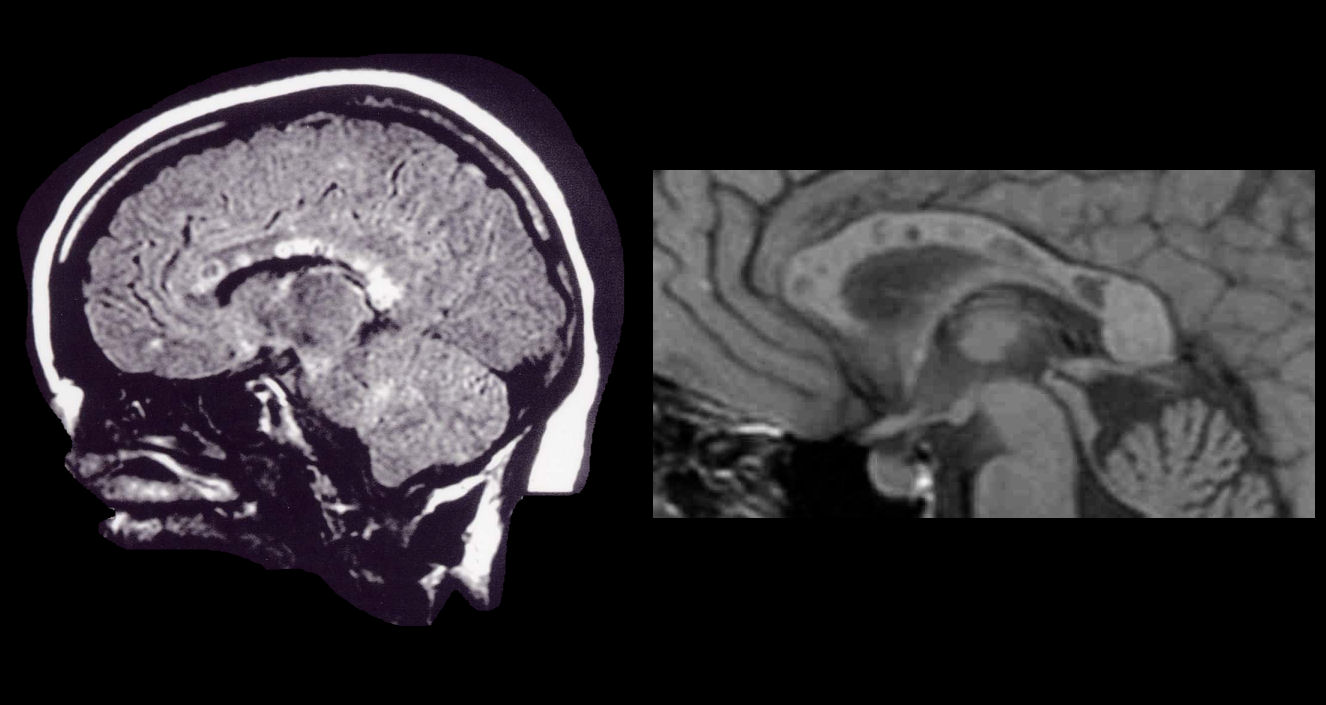
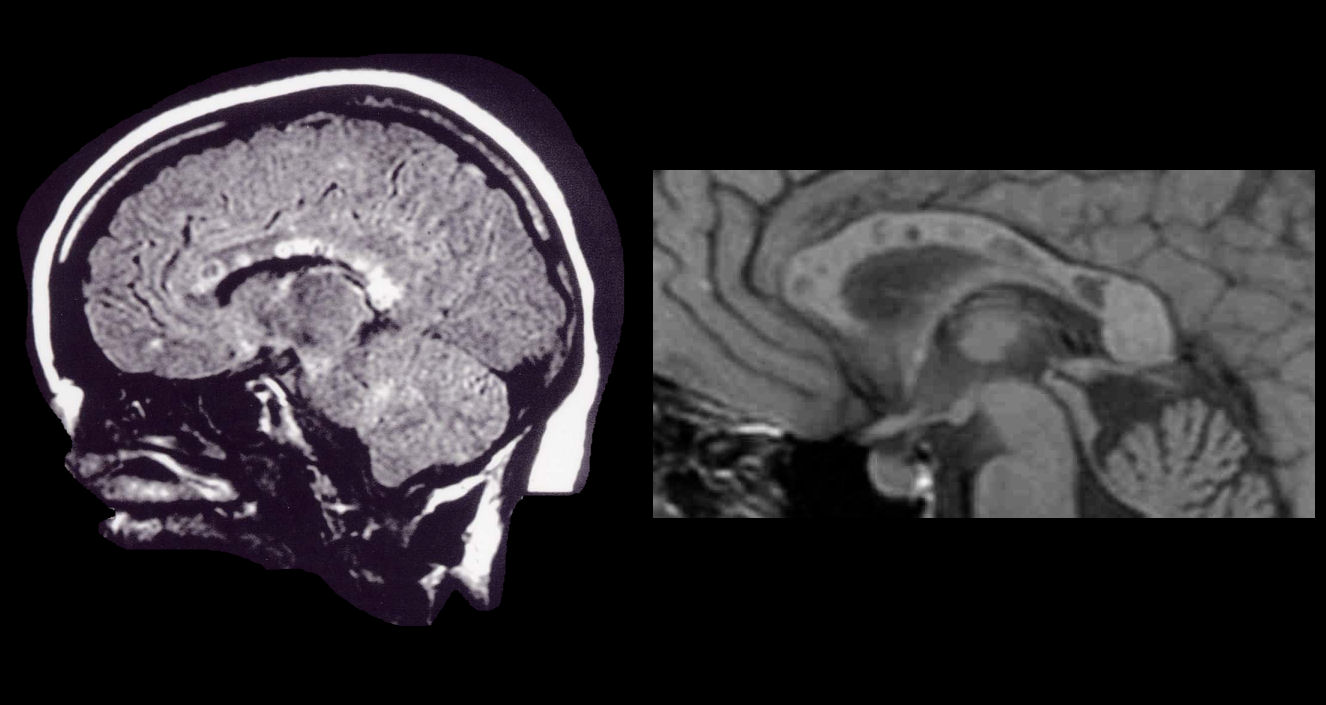
MRI Sagittal Images: (Left) Flair, (Right) T1-weighted with close up of the
corpus callosum. Note the prominent involvement of the corpus callosum. On the
close up of the corpus callosum, note the the prominent black holes (pictures
courtesy of John O. Susac, MD).
Susac's Syndrome is a rare neurologic syndrome with a clinical triad of encephalopathy, branch retinal artery occlusions, and hearing loss. The encephalopathy usually evolves subacutely and is frequently associated with headache and psychiatric features (especially personality change and bizarre and paranoid behavior). It may progress to a stage where the patient is totally unable to communicate. Seizures and myoclonus may occur. In other cases, patients may present with prominent brainstem/cerebellar signs. Hearing loss is usually bilateral, is often associated with tinnitus and vertigo and may be the presenting feature of the illness.
The MRI is the diagnostic procedure of choice. The white matter, especially the corpus callosum, is always involved. In addition to the white matter, the gray matter is frequently affected and gadolinium enhancement is seen in approximately three-fourths of these patients. Spinal fluid examination has invariably shown an elevated protein in the range of 100 mg to 3 grams. A minimal pleocytosis is seen occasionally.
Because the affected vessels are less than 100 um, cerebral angiography is almost always normal. Likewise, laboratory testing for collagen vascular disease, coagulopathy, infectious disease, including syphilis and Lyme disease, is unrevealing. The sed-rate may be elevated in a minority of cases. The EEG will be diffusely slow in the encephalopathic phase. The clinical course is self-limited, ranging from one to four years, but usually lasts from two to four years in most cases. During this fluctuating clinical course, the patient may have had one or more episodes of the triad but there is a definite remission noted at four years. Approximately one-half of these patients are able to return to an essentially normal lifestyle, but the others are left with a mild to moderate dementia.
Although the pathogenesis of this syndrome is unknown, an autoimmune basis is felt to be likely. Brain biopsies have shown perivascular inflammation of small vessels and microinfarctions of the brain. Necrosis is not found in the vessel walls and therefore it is a vasculopathy (microangiopathy) rather than a vasculitis. Recommended treatment consistent of intravenous methylprednisolone, followed by oral steroids in conjunction with the use of intravenous immunoglobulin (IVIG). In some cases, cyclophosphamide is used in addition.
Revised
02/03/05.
The Electronic Curriculum is copyrighted 1998, Case Western Reserve University
School of Medicine.