| |
|
Clinical Differentiation:
Cortical vs. Subcortical Strokes
|
|
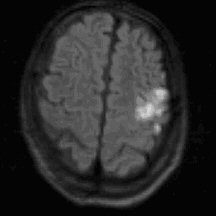
Cortical |
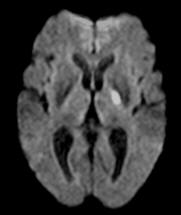
Subcortical |
A stroke may affect cortical regions of the cerebral cortex, including the
frontal, parietal, temporal and occipital lobes, or structures subcortically,
below the cortex, including the internal capsule, thalamus, basal ganglia,
brainstem and cerebellum. This differentiation is clinically important as the
etiology and clinical management of cortical and subcortical strokes may differ.
For instance, a distal branch middle cerebral artery occlusion resulting in a
cortical stroke usually results from an embolus from either the heart, aortic
arch or carotid artery, whereas a tiny infarct in the internal capsule is
usually due to
a blockage of small penetrating artery (lacunar infarct).
Cortical strokes may disrupt higher cognitive function. Depending on
the side of the brain and the lobe involved, different functions are impaired.
For example, a left MCA stroke to the inferior frontal lobe may result in an
expressive aphasia, an inability to express language. It is uncommon for
subcortical strokes to affect language (note: dysarthria is not a language
disturbance). A dominant posterior cerebral artery stroke may result in pure
alexia, a disturbance of reading. Other disturbances such as agraphia, an
inability to write, and acalculia, a disturbance of calculation may occur with
dominant cortical strokes. Right parietal strokes may result in a neglect
syndrome, a denial of deficits and stimuli on the contralateral body, or
difficulty in spatial organization which results in impaired drawing, copying or
interpreting pictures. It is rare for a subcortical stroke to disrupt these
higher order mental functions.
Motor and sensory impairments can be helpful in differentiating a cortical
versus subcortical location of stroke. With cortical sensory or motor deficits a
characteristic distribution is observed which is referable to the homunculus of
the cortex (figure below). |
 |
The result is preferential involvement of different motor areas. For example, a
left MCA stroke will often result in a motor deficit involving the right face
and arm more than leg, while a left ACA stroke will affect the right leg more
than face and arm. Focal weakness of a distal extremity may occur as well. In
contrast, a subcortical stroke presentation may involve face, arm and leg to an
equal extent. This is based on the close proximity of corticospinal tract fibers
to each other as they run through the subcortical structures such as the
internal capsule and brainstem. When primary sensation is impaired due to a
cortical stroke, it follows a specific distribution based on the topographical
representation of the homunculus. Thus, it would be unusual for a cortical stroke
to involve the entire contralateral hemibody. However, it is not uncommon for a
small subcortical thalamic infarct to result in hemisensory face, arm and leg
impairment.
The type of sensory loss from a cortical stroke may present differently from
subcortical sensory impairment. More specifically, a cortical stroke may result
in loss of higher order sensory function. For example, with a parietal stroke,
the patient may have contralateral agraphesthesia. This refers to loss of the
ability to recognize a number or letter traced on a limb, despite intact
sensation to the limb. Astereognosia may occur with cortical stroke, which is a
loss of ability to recognize objects by touch, despite intact primary sensory
sensation.
Lesions of the cortex may result in visual disturbances. For example,
occipital lobe infarcts will result in disturbance of vision in the
contralateral visual field. Similar deficits can occur with cortical strokes
affecting the temporal and parietal lobes where the optic radiations travel.
Other more complex, cortical visual abnormalities may be seen with occipital
lobe strokes such as palinopsia, which is a persistence of visual perception of an object
after an object is removed. It is rare for a subcortical stroke to impair
vision.
Cortical stroke may present with a gaze preference. This occurs when the
frontal eye fields, responsible for horizontal gaze, are infarcted. The result
is that the patient’s eyes will deviate to the side of the stroke. For example,
a right cortical stroke will result in a patient’s eyes being deviated to the
right side. This results from the unopposed action of the left frontal eye
fields on horizontal gaze to the contralateral right side.
Lesions which are subcortical in the brainstem may present with signs and
symptoms such as extraocular movement impairments, diplopia, dysphagia,
dysarthria, nystagmus. A subcortical stroke in the cerebellum may present with
nausea, vomiting, vertigo, imbalance. Exam may reveal nystagmus, ataxia and
tremor. |
TABLE: Clinical Distinction of Cortical and Subcortical Strokes* |
|
Higher Mental Functions:
Aphasia
Alexia
Agraphia
Acalculia
Neglect
Visual spatial disorientation
Memory impairment
Behavioral change
Visual disturbance:
Homonymous hemianopia
Gaze preference
Motor involvement:
Focal motor weakness
Face/Arm > Leg or Leg > Face/Arm
Face = Arm = Leg
Sensory involvement:
Agraphesthesia/Astereognosia
Focal sensory loss
Hemi-sensory loss
Brainstem findings
(see above text for examples)
Cerebellar signs:
(see above text for examples)
|
Cortical
x
x
x
x
x
x
x
x
x
x
x
x
x
x
|
Subcortical
x
x
x
x |
|
* Please note that the above table lists general guidelines. Exceptions may
occur.
|
|
|
|