|
RECOGNITION OF SPONTANEOUS
CAROTID OR VERTEBRAL ARTERY DISSECTION |
|
Although generally rare, dissection of the carotid and vertebral arteries
comprises a substantial number of
strokes among young adults and middle-aged patients.
The recognition of a spontaneous carotid or vertebral dissection requires a high
degree of clinical suspicion and an ability to recognize some key neurological
signs which help to hone in on the diagnosis. Dissection is critical to detect
before ischemia occurs so that treatment can be initiated promptly.
Arterial dissection occurs due to a tear in the intimal layer of the artery. The
tear allows blood to enter the wall and form an intramural hematoma. Depending
on which layer of the blood vessel is involved, either a subintimal or a
subadventitial hematoma develops. A subintimal hematoma tends to cause stenosis
of the artery, whereas a subadventitial hematoma often results in aneurysmal
dilatation of the artery. In the case of stenosis, sluggish blood flow distal to
the dissection results in the formation of fibrin clot. The clot continues to
enlarge and eventually breaks off to travel and dislodge downstream as an
embolus.
|
|
|
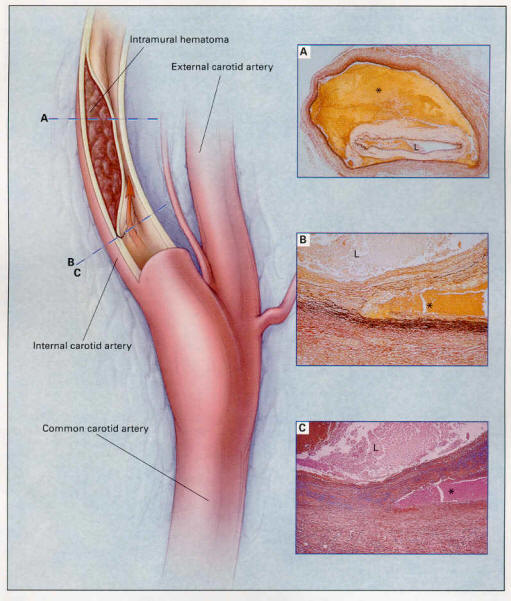
Above Figure: Pathological Findings in a
37-Year-Old Woman with a Dissection of the Internal Carotid Artery.
Photomicrographs of the right extracranial internal carotid artery (Panels A, B,
and C) show a dissection within the outer layers of the tunica media, resulting
in stenosis of the arterial lumen (L). The rectangles outlined in blue on the
left indicate the sites of the photomicrographs. The intramural hemorrhage
(asterisk) extends almost entirely around the artery (Panel A) (van Gieson's
stain, x4). Higher-power views of the internal carotid artery at the point of
dissection show fragmentation of elastic tissue (Panel B) (van Gieson's stain,
x25), with the accumulation of pale ground-glass substance in the tunica media,
indicated by the blue-staining mucopolysaccharides (Panel C) (Alcian blue, x25).
These changes are consistent with a diagnosis of cystic medial necrosis. From
Schievink et. al, Current Concepts: Spontaneous Dissection of the Carotid and
Vertebral Arteries, NEJM, 344 (12): 898, Figure 1, March 22, 2001.
|
|
Etiology
Most dissections involve some type of trauma or stretch to the head or neck
Sometimes, the trauma is trivial and forgotten by the patient
Higher incidence in certain congenital connective tissues disorders,
including Marfan's syndrome, cystic medial necrosis, and fibromuscular dysplasia.
|
|
Carotid Artery Dissection: Symptoms and Signs
The classic symptoms and signs of carotid dissection include the following:
• Pain or headache on one side of the head, face
or neck.
Headache (60-75%)
Usually unilateral
frontotemporal area
Of the patients with headache,
it is the initial symptom is 47%
Headache is described as severe
in 75%; mild-to-moderate in 25%
Headache onset is gradual in
85%; acute in 15% (and can mimic the presentation of SAH)
• Unilateral neck pain (25%), usually upper
anterolateral cervical region |
|

|
|
• Partial Horner’s syndrome (58%). Patients
develop ptosis and miosis (see figure above) as the sympathetic fibers to the
eye runs in the carotid sheath.
• Pulsatile tinnitus (27%)
• Cranial nerve palsies (12%), usually IX to XII;
impaired taste in 10%
• Cerebral or retinal ischemia
Cerebral hemispheric stroke or
TIA in the anterior circulation or
retinal ischemic symptoms (50-95%)
Transient monocular blindness
(25%)
TIA or transient monocular
blindness preceding stroke in 10-50% |
Vertebral Artery Dissection: Symptoms and Signs
Typically presents with the following:
• Pain in the back of neck, although can be
diffuse or frontal. Median interval between neck pain and ischemic symptoms is 2
weeks.
• Headache (median interval from onset of
headache to ischemia is 15 hours)
Headache occurs in 66%, usually
ipsilateral to dissection, and located in the occipital or frontal areas
Pain in back of neck (50%)
• Ischemia of
the posterior circulation (>90%).
Brainstem signs
Wallenberg’s syndrome |
Evaluation
Once the diagnosis of dissection is suspected,
fat-suppression MRI is the imaging study of choice. Intramural blood
can be well demonstrated on these scans. Routine Magnetic resonance angiography
(MRA) will often demonstrate narrowing or occlusion of the vessel, but in most
cases cannot differentiate dissection from other etiologies. |
|
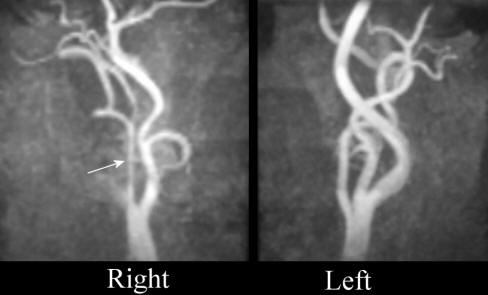 |
Above: Magnetic Resonance Angiogram - Both
Carotid Arteries - note the "string sign" of the right internal carotid,
compared to the normal image of the left internal carotid artery. Although not
specific for dissection, this pattern is highly suggestive
|
|
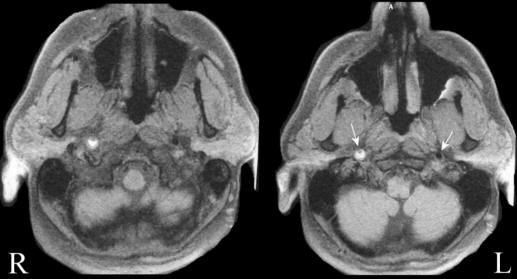 |
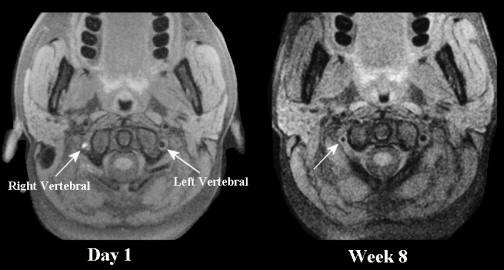
Above: MRI - Axial images of the lower
brainstem - fat suppression images (i.e., dissection protocol) - notice the
normal flow void (black signal in the left internal artery) and the bright
signal surrounding the right internal carotid area with a small lumen inside.
The bright signal is blood, indicating a dissection of the carotid artery.
|
|
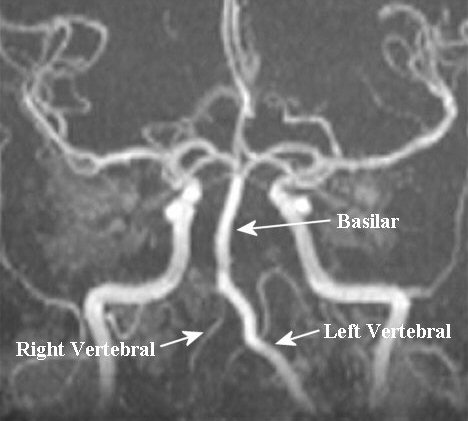 |
Above: Magnetic resonance angiogram of the
posterior circulation. Note the normal caliber of the left vertebral and basilar
arteries. However, the right vertebral is poorly seen, only a small amount of
flow is seen. This picture could result from a congenital hypoplastic vertebral
or from a dissection and a subsequent "string sign".
|
|
 |
Above: Axial MRI imaging with fat
suppression (i.e., dissection protocol). Notice the normal flow void in the left
vertebral artery. However, the right vertebral artery is poorly seen. The area
of bright signal represents blood inside the vessel wall from the dissection.
|