| |
|
|
COMPLETE TRANSECTION |
|
|
|
Complete transection of the spinal cord results in a devastating
neurologic injury. The most common etiologies include
trauma; compression from tumor, hematoma, or
abscess; or
transverse myelitis
(viral, post-viral, or demyelinative), among other causes.
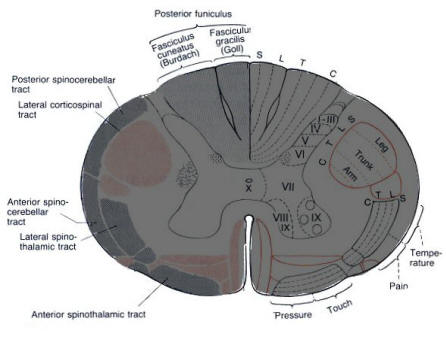
Transection of the spinal cord results in interruption of the long motor and
sensory tracts with concomitant complete loss of voluntary motor and sensory
function below the level of the transection. Below the
level of the lesion, the deficit will display an
upper motor neuron syndrome
(UMN) from interruption of the descending corticospinal tracts. However, at the
exact level of the transection, there will be local damage to the anterior horn
cells, its adjoining motor roots, and the nearby sensory roots.
This leads to a lower motor neuron (LMN) picture at the
level of the lesion. In many cases, this band of LMN damage may be
difficult to discern on physical examination.
Minutes after a complete cord transection, there follows a period of spinal
cord hypoexcitability referred to as "spinal shock,"
which may last days to weeks. During this period, there is complete absence of
reflex and autonomic activity below the level of the injury with flaccid
paralysis. When the stage of spinal shock passes, the typical UMN picture within
hyperreflexia and spastic paralysis below the level of the injury supervenes.
Clinical symptoms and signs of spinal cord transection depend on the level
injured. There are several locations and their respective patterns to be
aware of:
|
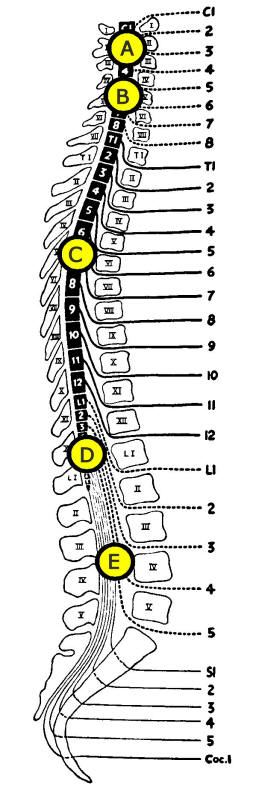
Levels of Spinal Cord Transection
A.
High Cervical
B.
Mid-Lower Cervical
C. Thoracic
E.
Conus Medullaris
F.
Cauda Equina |
A.
High Cervical Cord Transection |
|
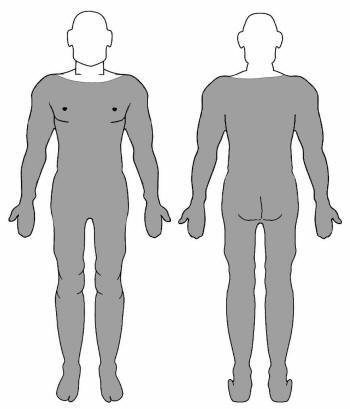
A high cervical injury results in quadriplegia and anesthesia below the level of the injury. In
addition, transection at the level of C2 results in sensory loss over the whole
body and the occipital area (indeed, all dermatomal regions except the
trigeminal nerve's sensory distribution). Lesions at the level of C4 and below
may allow for enough preserved phrenic nerve function (C3, C4, and C5) to allow
for adequate diaphragmatic function after the period of acute injury. However,
lesions at C3 and above are associated with acute respiratory collapse.
During the initial stage of spinal shock after cord transection at any level,
reflex emptying of the bladder may be lost, resulting in urinary retention and
bladder distention. In lesions that occur above the sacral level leaving the
spinal bladder center in the conus medullaris intact, automatic, reflex emptying
of the bladder returns days to weeks after the injury. Similarly, bowel function
ceases immediately after complete cord transection at any level, with loss of
rectal tone and the anal "wink" reflex. Spontaneous bowel peristalsis returns
within a few days as a rule, as do the anal and bulbocavernosus reflexes when
the cord lesion lies above the sacral level. Constipation and sexual dysfunction
are common. Later, in the hyperreflexic stage, anal tone may actually become
significantly increased.
|

B. Mid-Lower
Cervical Transection |
Lesions from C6 to T1 involve diminishing subgroups of the muscles innervated by
the brachial plexus and allow for increasing function of the arms and hands. In
general, the shoulder girdle muscles are supplied by C5-6; the elbow and wrist
flexors by C6-7; the elbow and wrist extensors by C7-8, and the hand muscles by
C8-T1. Horner's syndrome (ptosis, miosis, anhidrosis, and absence of facial
flushing) may be seen in cervical cord transection above the level of T1 owing
to disruption of descending sympathetic fibers. Full diaphragmatic innervation
compensates for loss of innervation of the intercostal muscles and other
auxiliary respiratory muscles.
In mid- and lower cervical transection, it may be
possible to identify the band of LMN at the level of the lesion
(above figure: blue areas). For instance, in a C6 transection, the biceps reflex
may be absent (LMN) with the triceps and finger flexors being hyperactive (UMN).
|

C. Thoracic
Transection |
Spinal cord transection below the level of T1 results in paraplegia but allows
for complete use of the upper extremities, including the hands. With lesions
above T6, the abdominal reflexes are lost. With lesions at T10, the upper
abdominal reflexes are preserved; with those at T12, all abdominal reflexes are
present.
|

D. Conus
Medullaris Transection |
Injury to the conus medullaris results in prominent bowel, bladder, and
sexual dysfunction. In these lesions that interrupt the bladder center, the
bladder becomes autonomous with feeble, inefficient, and uncoordinated
contractions of the detrusor muscle. As the conus medullaris contains UMN fibers
rostally, and LMN fibers caudally, patients may exhibit either UMN or LMN signs.
Signs are almost identical to those of the cauda equina syndrome (see below),
except that in conus medullaris injuries, signs are more likely to be bilateral
(due to the fact it is such a small area). Combinations of a spastic and atonic
bladder may occur in partial cord lesions.
|
|

E. Cauda
Equina Transection |
|
Although the cauda equina is not the spinal cord, per se, it is best considered
here. Because the cauda equina is composed of the lumbosacral roots as they
descend into the thecal sac below the termination of the spinal cord, pathologic
processes in this area result in lower extremity weakness and paralysis
(depending on the level of the lesion) along with sensory loss. So-called
"saddle anesthesia" is often prominent representing the sensory territory of the
sacral roots (above figure - dark gray). Similar to conus medullaris lesions,
bladder and bowel dysfunction may be prominent.
Please note: the cauda equina syndrome always displays LMN signs (hypo- or
areflexia and hypotonia).
|
|
|
|